Could the Gut Microbiome be Linked to Autism?
Researchers are hoping to understand whether the microbes in our guts have a role in the disorder.

Before Ethan Loyola reached his first birthday, it was clear that something was wrong with his gut. As a baby, he had been given several courses of antibiotics to treat severe ear infections, after which he experienced foul-smelling, acidic diarrhoea that left him convulsed with pain. Around the age of one, Ethan lost the words he’d started to say and stopped making eye contact. Soon after that, he received a diagnosis: autism spectrum disorder (ASD).
As Ethan grew older, his digestive issues continued, and he struggled around other people and in unusual situations. “He had his hands over his ears, didn’t want to be in crowds,” says his mother, Dana Woods. “It was just too overwhelming.” Then Ethan’s dad saw a flyer tacked up at an autism therapy clinic. Scientists at Arizona State University in Tempe, near the family’s Phoenix home, were looking for children with autism to try an experimental treatment called microbiota transfer therapy, which would be used to recolonize the children’s guts with bacteria from donors who were not on the autistic spectrum. Ethan’s parents enrolled him in the study.Part of Nature Outlook: The gut microbiome
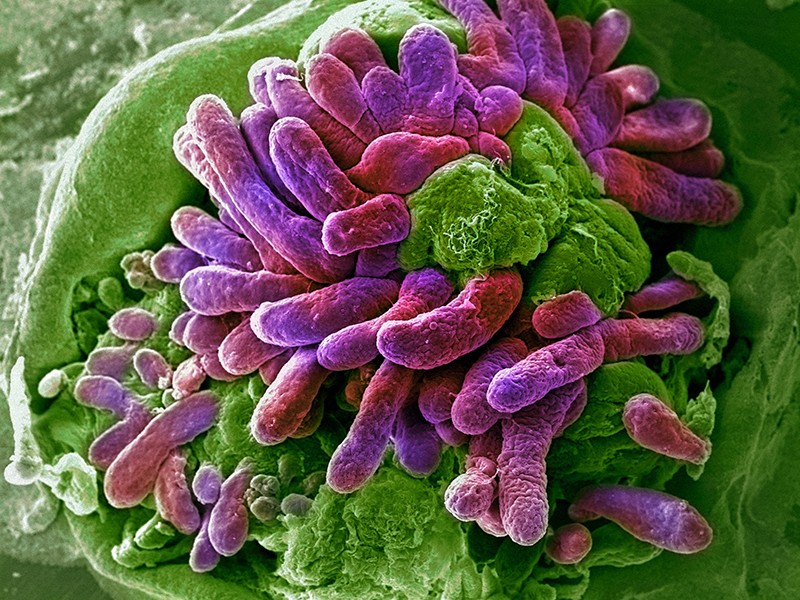
ASD can cause various language and social difficulties. And, for the 1 in 160 children it affects worldwide, treatments have been frustratingly slow in coming. Some parents have long claimed that changing a child’s diet or giving them probiotics improves not just digestive problems, but also behavioural symptoms. Now, researchers are revealing that in addition to aiding digestion, gut bacteria also manufacture bioactive compounds that help to orchestrate brain function and social development. Studies show that children with ASD often have a mix of gut microbes that is distinct from that in children without the condition. And in lab animals, autism-like symptoms arise when normal species of gut bacteria are absent.
Although far from conclusive, these findings are driving researchers to probe the links between gut microbes and autism symptoms — and to begin testing ASD treatments that repopulate the gut microbiome from scratch.
Laying gut groundwork
John Cryan, a biochemist at University College Cork in Ireland, was among the first researchers to investigate how gut microbes affect social behaviour. In 2014, he reported that germ-free mice — those lacking the typical mix of gut microbes — avoided other mice, shunned new social situations and groomed themselves excessively1. “It started to crystallize that the microbiome was involved in many aspects of behaviour,” Cryan says. “There seems to be something about the social brain in particular that makes it sensitive to signals from the microbiome.” He and other scientists proposed the existence of a gut–brain axis, in which gut microbes produce bioactive compounds that influence brain function.
Other studies have bolstered this theory, showing that when gut bacteria help to digest food, they generate a host of by-products that can affect thinking and behaviour. Clostridia bacterial pathogens, for instance, generate propionic acid in the gut — a short-chain fatty acid known to disrupt the production of neurotransmitters. Propionic acid also causes autism-like symptoms in rats, such as repetitive interests, unusual motor movements and atypical social interactions2.
Deficits in beneficial gut bacteria might also affect social brain function. In 2017, Cryan reported that when mice with an autism-like condition had lower levels of Bifidobacterium and Blautia gut bacteria, their guts made less tryptophan and bile acid — compounds needed to produce serotonin3. And children with autism have been consistently found to have lower levels of Veillonellaceae, Coprococcus and Prevotella gut bacteria than those without the condition4. Researchers have also observed that some people with ASD could have an abnormally porous blood–brain barrier, which allows some toxic bacterial by-products to enter the bloodstream and reach the brain5.
Behavioural change
Such findings prompted researchers at the California Institute of Technology in Pasadena to transfer the microbes of people with ASD into mice. Microbiologist Sarkis Mazmanian and his colleagues gave germ-free mice gut microbes from people with ASD; at six weeks old, offspring of these mice socialized less, produced fewer vocal sounds and engaged in more repetitive behaviour, compared with mice descended from animals that received gut microbes from donors who did not have ASD6.
The differences between the two groups also proved striking on a biological level. “We uncovered several differences in faecal and serum metabolites,” says Gil Sharon, a co-author of the research. In particular, mice with gut microbes from donors with ASD had lower levels of compounds produced by gut bacteria that are thought to affect brain function. In particular, the amino acids 5-aminovaleric acid (5AV) and taurine were depleted — both metabolites increase the activity of the brain’s γ-aminobutyric acid (GABA) receptors. GABA is a neurotransmitter involved in sensory processing and motor control, and abnormalities in the GABA system have been noted in children with ASD.
When the team gave the two missing metabolites to mice with autism-like symptoms, Sharon says, “they improved core deficits in social interaction and repetitive behaviour”. The study has received some criticism regarding its data analysis and small sample size. The finding that mice with microbes from donors with ASD vocalized less, one critic argued (see go.nature.com/2qbqwy1), involved gut bacteria from only five donors with autism and three without, and the researchers ran many analyses on the data to find a difference between the two groups of mice — the more analyses run on a data set, the more likely it is that a false effect could be found. The team declined to comment on these criticisms, but stands by its results.
The growing focus on the role of gut microbes in social brain function prompted the team at Arizona State University to up the ante by testing microbes in children with ASD. Microbial ecologist Rosa Krajmalnik-Brown and her colleagues recruited a group of 18 children with ASD aged between 7 and 16, including Ethan Loyola. Like Ethan, all of the children had a history of gastrointestinal problems, including chronic diarrhoea, pain and constipation.
The children in the study took the antibiotic vancomycin for two weeks to remove existing bacteria. Then, each of them received a high dose of gut microbes from donors without autism — some children received this as an enema, whereas others took a bacteria-fortified drink. The children continued to take a daily dose of microbes for seven or eight weeks (Ethan took his in a shot glass, mixed with cranberry juice), along with an antacid to neutralize stomach acid and improve the chance of the new microbes surviving.
At the end of the 18-week study period, the children’s gastrointestinal symptoms had reduced by 80%, and most of the improvement remained two years after the original study. By the two-year mark, the children’s scores on a test to measure how much they were affected by their autism were an average of 47% lower than they had been at the beginning of the trial. Also at the two-year follow-up, the children had increased gut-bacterial diversity and greater numbers of gut bacteria that are often found in lower numbers in children with ASD, such as Bifidobacteria and Prevotella. This suggests that the treatment had succeeded in changing their microbiomes long term, Krajmalnik-Brown says.
A muddled outlook
Although these early results look promising, the authors stress that little will be known for sure until they complete a larger trial that includes a control group. “The fact that we have exciting results doesn’t mean that this will work for everyone,” Krajmalnik-Brown says. Her team is now carrying out a phase II trial of microbiota transfer therapy with 84 adults with ASD, some of whom will receive a placebo. The team is also looking for funding to start a similar trial in children. And even if these trials are successful, even bigger phase III trials will be needed a few years down the line before the treatment can be used in the clinic. Along the way, Krajmalnik-Brown’s team is hoping to work out the biological mechanisms behind the improvement in symptoms.
There is currently no approved medication specifically for the core symptoms of autism — communication difficulties, social challenges and repetitive behaviour. Krajmalnik-Brown hopes that her research will lead to one, but this is by no means assured. Although studies report that people with ASD have a gut-bacterial profile distinct from that of people without the condition, no study has yet shown that gut microbes cause autism in people. One leading hypothesis is that some microbes could cause autistic symptoms to be worse in people who are prone to the condition, but this too remains unproven. People with ASD might harbour different gut microbes from those without the condition because they tend to have very specific dietary preferences.
Likewise, evidence that gut microbial therapies can help people with ASD is mixed. Krajmalnik-Brown strikes an optimistic note, but a review of four other studies did not reach a clear conclusion about the benefits of gut bacterial supplementation in children with ASD — although these earlier studies used ordinary probiotics and not bacteria directly from the human gut7. “The human data is very heterogeneous,” Cryan says. “If we target the microbes, it will be interesting to see if we have behavioural effects, but we need more evidence overall.”More from Nature Outlooks
As Krajmalnik-Brown’s trials progress, she warns children and families to steer clear of do-it-yourself faecal transplants. Instead, she says they should discuss options for altering the balance of gut microbes, such as conventional probiotics, with their physician. She also wants to temper people’s expectations for the treatment. “This might help alleviate the symptoms. I don’t believe that we have a cure on our hands,” she says.
For Ethan, however, the Arizona State study resulted in a striking turnaround. After the microbiome transfer, his diarrhoea and cramping disappeared in months. But most dramatic was his new interest in people. He began waking up with a smile, crowing, “Good morning!” He also started asking questions, such as ‘why is the sky blue and the clouds white?’ something he had not done before, his family says. In social-skills tests, Ethan, who is now 12, scores in the same range as children who are not on the autistic spectrum.
Did Ethan make these strides because his crippling stomach pain went away? Or have the new microbes truly changed the way his brain works? No one knows for sure. But Ethan’s family welcomes the research. “The study was the tipping point,” his mother says. “It was completely life altering.”
Looking forward, Cryan says, it’s crucial for scientists to keep decoding the biological pathways that connect the gut to the brain. “We’re optimistic that a healthy gut will mean a healthy brain, but we need the data.” Those data should help to determine just what fuelled Ethan’s improvements — and whether thousands of other children could follow a similar course.
Nature 577, S14-S15 (2020)